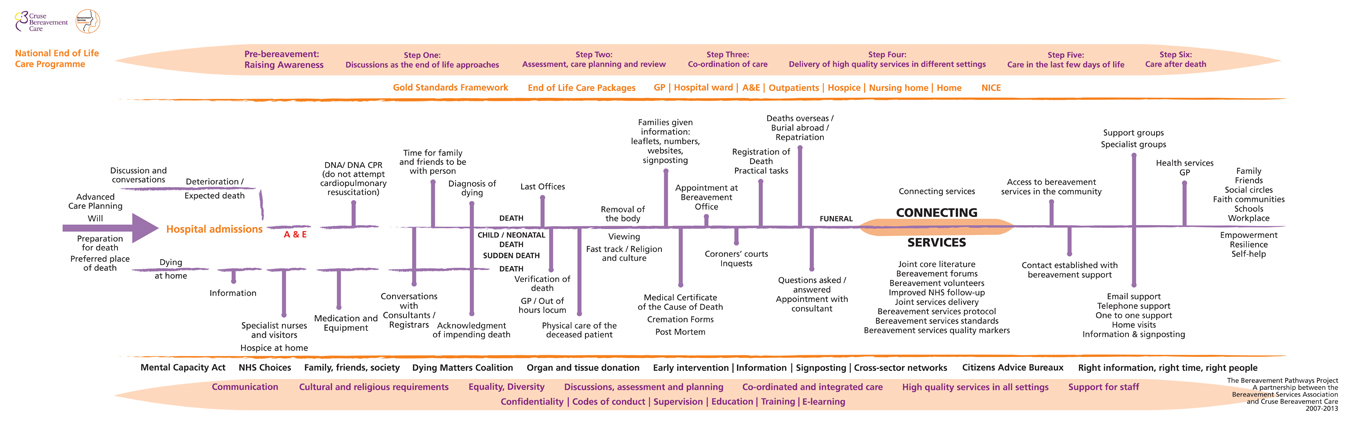
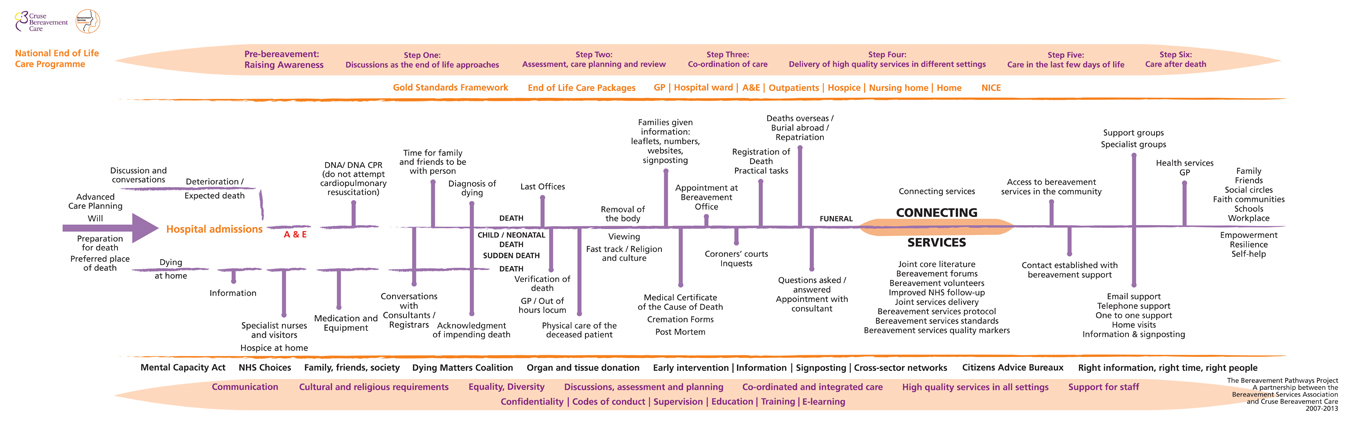
The 'Bereavement Pathway' is grouped in rough order from the time of diagnosis of a life-threatening condition (left) to the time after someone has died (right).
To access the information and links, please click on the entries to open a new information box.
It is important to remember that end of life care issues are not only the concern of specialist palliative care hospital staff. People approaching their life's end can be cared for in a variety of settings by a variety of professionals and volunteers from both the statutory and voluntary sectors. While death may be expected, it may also be sudden and affect people st any age.
It is important for all involved in offering care in whatever setting to be aware of high quality practice in end of life care and put that into practice.
It is also important to remember that there is a wide difference of beliefs and practice within faiths and cultures – and within families. It is always appropriate to ask what forms of care would be appreciated and when.
Those providing care after death need to be aware of traditions associated with the treatment and disposal of the body of the deceased person and the likely difficulties for some cultures if, for example, a post-mortem and/ or inquest is required and the funeral delayed.
Some faith traditions (for example, Islam and Judaism) will hold the funeral with little delay (within 24/ 48 hours). If there is no need for a post-mortem, any help in quickly providing documentation for registering the death will be appreciated.
The Multi-faith Group for Heath Care Chaplaincy has resources and information on its website.
Health care chaplains within the NHS can access faith-appropriate support (including secular/ humanist support) for patients and families.
It is also important to remember that there are many types of cultures, not all which are based around belief or ethnicity. For further reading on this:
Death and Bereavement across Cultures: Murray Parkes C. (editor); Routledge; 1996
On Bereavement; Culture and Grief: Walter T.; Open University Press; 1999
www.mfghc.com/resources/resources_faithindex.html
The National Institute for Health and Care Excellence (NICE) offers guidance on quality standards in end of life care.
All staff and volunteers in whatever setting (hospital, hospice, home, community bereavement service) should provide respectful care to the deceased person after death and to their grieving family and friends and carers. See details of core skills in the document.
Most of the information on this 'pathway' assumes an adult patient who is able to plan for their own death. However, sadly, children also die sudden or expected deaths and it is important that end of life care for children and young people is of as high quality as that for adults.
Many organisations offer support to families when a child is expected to die or has died. These include (web links below)
Together for Short Lives supports children with life-threatening and life-limiting conditions and all those who support, love and care for them in a range of services, including children's hospices: 0808 8088 100
The General Medical Council's guidance on end of life care carries a section about child and neonatal death.)
SANDS (the Stillbirth and Neonatal Death Charity) supports families when a baby dies at and just after birth: 020 7436 5881 Email helpline@uk-sands.org
The Lullaby Trust provides support to families and anyone affected by a sudden infant death: 0808 802 6868
Child Death Helpline offers support to anyone affected by the death of a child of any age from whatever cause: 0800 282986 or 0808 800 6019 from mobiles
Cruse offers support (telephone, email, face to face) to everyone affected by a death, regardless of the age of the person: 0844 477 9400 Email helpline@cruse.org.uk
Child Bereavement UK offers support to anyone caring for children when a sibling has died and also to grieving parents after the death of a baby or child: 0800 02 88840 Email support@childbereavementuk.org.uk
Winston's Wish offers support to anyone caring for a child when a sibling has died: 08452 030405 Email chris@winstonswish.org.uk
http://www.togetherforshortlives.org.uk
http://www.togetherforshortlives.org.uk/assets/0000/1089/End_of_life_planning_family_factsheet.pdf
http://www.gmc-uk.org/guidance/ethical_guidance/end_of_life_contents.asp
http://www.bliss.org.uk/help-for-families/bereavement
http://www.lullabytrust.org.uk
http://www.childdeathhelpline.org.uk
Child death review process in England http://www.education.gov.uk/childrenandyoungpeople/safeguardingchildren/childdeathreview and Wales http://www.wales.nhs.uk/sitesplus/888/page/44351
Wales http://www.wales.nhs.uk/sitesplus/888/page/44351
Fatal accident inquiries in Scotland need to link to http://www.scotland-judiciary.org.uk/10/0/Fatal-Accident-Inquiries
Confidentiality is the underlying principle that makes most therapeutic relationships work. It is based on trust and the limits to confidentiality (if any) practiced by any statutory or voluntary organisation should be openly shared with those it is supporting. Broadly speaking, most of those organisations offering support to family members after a death will protect confidentiality of what is being said as long as there is no threat to the life of the person being supported or to the life or safety of someone else. Some organisations may promise complete confidentiality, regardless of what is shared.
Any organisation should provide on request a copy of its confidentiality policy. In addition, the General Medical Council has guidance for members of the medical profession and the NHS has a briefing document for staff on how to put the principle of confidentiality into practice.
www.gmc-uk.org/guidance/ethical_guidance/confidentiality_contents.asp
www.england.nhs.uk/wp-content/uploads/2013/06/conf-policy-1.pdf
There can be great comfort for families and friends to view the deceased's body; some cultures may expect it to be possible. Family or friends who were not present at the time of death may wish to 'say goodbye' and those who were may need to see the body several times before the funeral in order to begin to understand what has happened.
If the death was within a hospital context, the mortuary will have a viewing room where the body can be brought. Hospices will have a 'quiet room' which is kept cool so that the body can remain in the room for some time.
Funeral services will also have arrangements for the person to be visited as often as the family requires before the funeral. However, usually this will involve an appointment since, in many cases, the person's body is held in a different location to the funeral office.
Some challenges arise when the death has been through accident or violence. Funeral directors and mortuary attendants are skilled in trying to make it possible for at least some part of the person to be viewed without causing unnecessary distress. Examples include revealing a hand or the lower part of a face. When identification needs to be made, it is not always possible to hide the effects and additional understanding and support is necessary.
It is always helpful for the family to be prepared for a viewing; practical details such as the warmth of the room and the chill of the body; the presence of flowers, even the colour of the painted walls can help prepare families for this difficult task.
Children who were not present at the time of death may find the opportunity to view their relative's body helps them begin to understand what has happened. Child bereavement organisations can provide information on making this process comfortable for all concerned by providing information on what will be involved.
www.nhsiq.nhs.uk/media/2426968/care_after_death___guidance.pdf>
www.winstonswish.org.uk/page.asp?section=00010001000200110004>
A stretcher draw sheet is placed under the deceased person's body to enable removal to a trolley for transportation to the mortuary. These trolleys may often be disguised to resemble laundry carts if transportation has to pass through areas where members of the public may be present.
Hospital mortuaries can arrange viewing of the body for other family members: this is usually in a specially designed room – not, as some fear, in the mortuary itself.
Hospices almost always have a 'quiet' room which is kept cool and where the deceased's body can remain for a period of time/days to allow family and friends to sit with them. Some hospices have offered their 'quiet' room to families where a death has occurred elsewhere (at home or in hospital).
The deceased body can remain at home if this is the family's wish for at least a couple of days. There is no legal requirement to move the body to a funeral director's premises or equivalent location.
When contacted, funeral directors can collect the deceased person's body within hours. It is also legal for families to transport their relative's body, for example between hospital or hospice and home, if that is desired.
www.nhsiq.nhs.uk/media/2426968/care_after_death___guidance.pdf
All those who are involved in supporting patients, families and friends, and staff are committed to providing the best possible care. Quality standards have been developed by professional organisations that help organisations monitor and ensure consistent high quality.
The End of Life Care quality standards developed by NICE can be accessed through the link below. The full list of NICE quality standards, including those under development, is also available.
Cruse Bereavement Care and the Bereavement Services Association, through the support of the Department of Health, have produced updated Standards in Bereavement Care Services.
Royal College of Emergency Medicine's End of life care for adults in the Emergency Department (February 2012) http://www.collemergencymed.ac.uk/Shop-Floor/Clinical%20Guidelines/default.asp
While everyone knows that they will die, few people actively think about the possibility of their impending death until they receive a terminal diagnosis. However, preparation for death (such as making a will, plans for guardianship of children, an Advance Care Plan) can help everyone feel more secure about the future: this is particularly true when someone is dying.
Being allowed to discuss fears can help the ill person to feel more in control and more able to face their future. Frequently, patients worry about pain control and about care at the end of life; realistic reassurance can be offered.
Organisations such as Dying Matters, Final Fling and the Death Café movement are encouraging the general population to discuss dying and death, recognising that only a relatively small proportion of people will know that they are dying before they die.
Preparing children and young people for a parent or sibling's expected death can have an impact on how they will experience bereavement. Guidance on talking to children can be found on the websites of Winston's Wish (who also produce a booklet called 'As Big As It Gets' for those supporting children before a parent's expected death) and Child Bereavement UK.
www.finalfling.com/sort-your-affairs
www.winstonswish.org.uk/page.asp?section=0001000100100002&pagetitle=As+Big+As+It+Gets
End of Life Care for All (e-ELCA) is an e-learning project aiming to enhance the training and education of health and social care staff involved in delivering end of life care to people, so that well-informed high quality care can be delivered by confident and competent staff and volunteers, across health and social care, wherever the person happens to be.
It delivers accessible, easily digestible e-learning materials in the 4 core modules of assessment, advance care planning, communication skills, and symptom management and maintaining comfort and wellbeing, regardless of the underlying condition.
Help the Hospices runs a large number of courses at different levels for those involved in palliative care, including e-learning packages.
A virtual learning/e-learning zone is also on the website of the Gold Standards Framework.
The Irish Hospice Foundation has also recently produced e-learning resources.
www.e-lfh.org.uk/projects/end-of-life-care
Grief is a natural response to the death of someone close.
Most people will find a way to live with their grief with the help and support of family and friends.
However, some people may lack this support or not want to trouble other people who are also grieving. It helps everyone who has been bereaved if they are automatically offered the chance to meet a bereavement support worker, either within a hospital or hospice or from a community bereavement service. Making an appointment makes it easier for the bereaved person to accept the support that may make a real difference.
Cruse offers free confidential support to adults, children and young people, and this can be by telephone, email or face-to-face with a Cruse volunteer. Cruse has a website specifically for children and young people – rd4u.org.uk
Guidance and support for anyone caring for a bereaved child can be found by calling the Winston's Wish helpline on 08452 030405 or the helpline of Child Bereavement UK on 0800 02 888 40. Local services for children who have been bereaved are listed in the directory on the website of the Childhood Bereavement Network.
www.rcpsych.ac.uk/expertadvice/problems/bereavement/bereavement.aspx
As part of Advance Care Planning, people usually express a preference on where they would like to die. For the majority of people this is in their own home – with appropriate care and support; although others feel they and their family will feel more supported in a hospice or hospital setting. In practice, around half the people who die each year, die in hospital.
It is always important to be clear that medical, financial and other resource constraints may make it impossible to meet people's preferences but, wherever possible, respect for people's choices should be honoured.
Advance Care Planning is the description for the process of discussing and planning ahead, for example in anticipation of some deterioration in a patient's condition. There are two specific but overlapping areas within Advance Care Planning:
Advance Statement/Statement of wishes. This is a statement of what the person DOES wish to happen in their care. These are not legally binding, but can be invaluable in determining and planning care and interventions. Sensitive discussion of advance care planning can help people begin to explore their ways of adapting to a new reality, a new 'normal'.
Advance Decision. This is a statement of what the person DOES NOT wish to happen in their care. When worded correctly and linked to an assessment of mental competency, it can be legally binding and strengthens the role of Lasting Power of Attorney to enable a nominated proxy person to make decisions about medical as well as social welfare.
www.gmc-uk.org/guidance/ethical_guidance/end_of_life_advance_care_planning.asp
www.nhs.uk/CarersDirect/moneyandlegal/legal/Pages/Advancedecisions.aspx
Ideally, everyone over 18 should have already made a will and should regularly review and update it through codicils. However, it may be that it is not until there is a reason to be considering the approaching end of life, that people write their will.
A will is the place to indicate what a person chooses to do with any assets they possess (property, money, possessions). It is also the place to record plans for guardianship of any children. The will appoints people to act as executors who are required to carry out the person's wishes (after clearing any debts or charges to the estate and any inheritance tax).
Normally, a will is drawn up and witnessed by a solicitor. This may be done for a low fee to a chosen charity through the charity Will Aid during November (suggested donation around £100). Alternatively, template will forms can be obtained from stationers or online; these still need to be witnessed and lodged securely.
It is important that executors know where to find the will after the death.
There is no requirement to share the contents of the will before the will-writer has died and while the will, after a death, becomes a publically-accessible document through the Probate Service, it is not a requirement for the executors to share the contents after a death (although they may choose to share with anyone concerned).
www.adviceguide.org.uk/england/relationships_e/relationships_death_and_wills_e/wills.htm
If the death happened within a hospital setting, staff will help with issuing documents and explaining procedures. In many hospitals, this will be handled by experienced staff within the Bereavement Service; otherwise, ward staff will help.
In some circumstances, it can take a while for documents to be prepared (for example, if the staff involved in the patient's care are not immediately available); in this case, an appointment should be made before the family leave.
This appointment provides an opportunity for the family to collect documents, including the Medical Certificate of Death, and any remaining belongings and to have an opportunity to talk with the bereavement staff and be introduced to sources of help in the community.
This can also be the opportunity to discuss arrangements for the body of the deceased person to be transferred to a funeral home or other location from the hospital mortuary.
In the event of post mortem procedures being required, or referral of the death to the Coroner, this appointment provides an opportunity to explain what is happening.
A funeral has different meanings for different people. It is an opportunity to say goodbye to the person who has died and to mourn their loss. It can also be an occasion to celebrate their life.
For those who are planning a funeral there are some questions to answer:-
What were the deceased person's choices about their funeral? Had they expressed a choice in their Advance Care Plan or other document? Will it be possible to carry out these wishes?
Did they wish to be buried or cremated? Will this be possible? For example, if the deceased person had a pacemaker, this will make cremation impossible unless it is removed beforehand. Also, under some circumstances, if an inquest is yet to be heard, a coroner can give permission for a burial but not a cremation.
What faith and cultural requirements need to be met? If a funeral is culturally required to take place as soon as possible, what support is available to help? For example, out-of-hours contacts at the local place of worship, coroner's office and registrars prepared to speed the registration process through out of hours wherever possible. What arrangements do local faith groups have in place to ensure the body of the person who has died is cared for according to faith practice?
Involve funeral directors/undertakers? For most people, involving funeral directors makes the process of caring for the body after death and arranging a funeral simpler at an emotionally demanding time. The deceased person may have put in place a pre-paid funeral plan, which will mean using the firm with which it is registered. Information on finding a funeral director can be obtained from the National Association for Funeral Directors or the British Institute of Funeral Directors and also from the Natural Death Centre .
It is possible to arrange a funeral (more easily involving cremation) without using a firm of funeral directors. As long as the paperwork authorising the funeral is in place (Registrar's Certificate or Coroner's Order for Burial), it is possible to make arrangements directly with crematorium and, for example, use private transport and friends to carry the body. There are certain conditions surrounding what covering the body needs to have before cremation. More information is available from the Natural Death Centre or the Good Funerals Guide.
What does a funeral cost? Costs increase depending on what type of coffin is uses; what vehicles are required for the funeral; how long the deceased's body is looked after by the funeral directors; arrangements for viewing the body; the cost of flowers and notices; celebrant's and pall bearers' fees; the arrangements for food and drink for mourners. Recent research suggests that the average cost – using a firm of funeral directors – is over £3000 and can be much higher.
It is possible to significantly reduce this cost if those arranging the funeral – or the deceased - do not wish to spend this much. Information is available from the Natural Death Centre and Good Funerals Guide.
For those on low incomes and in receipt of certain benefits, there is a Funeral Payment available from Government. This covers basic costs and may need to be repaid in part or in full if the deceased has left an estate..
Should children attend funerals?Families, and individuals within families, can have very different views on whether children should see the person's body after death or attend the funeral. Families will have different cultural and religious beliefs about seeing the person who has died and attending the funeral, but it can help a child to:
Probably the biggest factor that will affect a younger child's attendance at a funeral is if they feel their presence is welcome there. If there is going to be tension (as distinct from sadness) they will pick this up and feel more distressed by the atmosphere than by what is happening. Many children understand and appreciate sharing in other people's sadness- after all it is what they are feeling too.
If it will not be possible or appropriate for children to attend the funeral, for whatever reason, there are other positive ways in which they can be involved. If the funeral happened a while ago and children have regrets that they did not attend, it is never too late to have a memorial or other ceremony that includes them saying 'goodbye'.
www.winstonswish.org.uk/funerals-and-other-memorials
When death is imminent, medical staff will recheck an Advance Care Plan to be guided by the person's expressed wishes about attempted resuscitation. Instructions about their choices should also appear on their medical notes, if the death is expected. There may be circumstances when medical staff decide to override a previously-lodged ACP; for example, if a person has more recently verbally expressed different instructions to medical staff.
Individual hospitals produce guidance on reaching and implementing DNAR decisions.
The 'Liverpool Care Pathway' is currently under evaluation; this had provided guidance to medical staff on the managed care of someone who was dying with no chance of recovery. The Leadership Alliance for the Care of Dying People are working rapidly to put in place guidance for staff on what should replace the LCP – this will involve processes to ensure that the focus is on individual choices and individual care.
www.england.nhs.uk/wp-content/uploads/2014/01/lacdp-interim-statement.pdf
www.gmc-uk.org/guidance/ethical_guidance/end_of_life_DNACPR_decision.asp
The National Council for Palliative Care (NCPC) set up the Dying Matters Coalition to promote public awareness of dying, death and bereavement. Members include organisations from across the NHS, from the voluntary and independent health and care sectors (including hospices, care homes, charities supporting older people, children and young people facing bereavement); social care and housing sectors; a wide range of faith organisations; community organisations; schools and colleges; academic bodies; trade unions; the legal profession and the funeral sector.
The Coalition's Mission is "to support changing knowledge, attitudes and behaviours towards death, dying and bereavement, and through this to make 'living and dying well' the norm". This will involve a fundamental change in society in which dying, death and bereavement will be seen and accepted as the natural part of everybody's life cycle.
The Dying Matters Coalition is working to address this by encouraging people to talk about their wishes towards the end of their lives, including where they want to die and their funeral plans, with friends, family and loved ones.
The key to providing the most helpful care to patients, to families and friends and to the professionals supporting them is sensitivity to what is the most appropriate response and the most appropriate time to offer this.
Well trained, intuitively caring supporters will know when to offer information and when to wait; when to leave people alone and when to ensure they are not alone; when to back away and when encouragement is necessary.
This comes instinctively but can be enabled and refined through training and through peer support and feedback.
The aim is that all concerned receive the right information at the right time from the right people.
Citizens Advice Bureaux deliver advice services from over 3,500 community locations in England and Wales, run by 382 individual charities. CAB also provide online advice on a huge range on issues, including what to do after a death and information about benefits and bereavement.
www.adviceguide.org.uk/england/benefits_e/benefits_bereavement_ew/benefits_and_bereavement.htm
The National Health Service is concerned with ensuring that all patients receive the highest quality of care from all NHS staff. The NHS Choices website carries guides for those who are caring for someone at the end of their life and for those who have been bereaved.
Gold Standards in Bereavement Care refers to a training programme (including e-learning) developed under this name for doctors, nurses and the staff of care homes.
People involved in caring for people who have life-threatening or terminal illness have developed 'pathways' with accompanying quality of care standards to ensure that the most appropriate care and support is offered to the person and their family and friends at the right time and in the right way.
The 'Liverpool Care Pathway' or LCP was the most used guide for care in the last days; however, this is currently undergoing review and being phased out after some concerns were raised about how some people may have interpreted the guidance provided. Links below provide up-to-date information about the LCP and about the Leadership Alliance for Care of Dying People.
The likely emphasis in the future is not to have a 'Pathway' as such, but to tailor response at the end of life to the needs and best care of individual people.
Other supportive care pathways (SCP) have been developed and are in operation. One example is the SCP developed by the Sandwell and West Birmingham NHS Trust. Like all such pathways, its underlying aim is to identify dying patients promptly and improve the quality of end of life care by providing a focus on end of life issues and ensuring the multidisciplinary team is closely involved at every stage. The pathway is not prescriptive and does not curtail any care that would benefit the patient. However, because it is an end of life care pathway, it will direct the team to consider comfort measures as a priority.
Local NHS Trusts can provide information on their own Supportive Care Pathway.
www.england.nhs.uk/wp-content/uploads/2014/01/lacdp-interim-statement.pdf
If the cause of death remains in doubt after a post-mortem examination and further tests are required, or if it is determined that the death was not from natural causes, an inquest will be held (in Scotland a 'fatal accident inquiry' although the circumstances in which a fatal accident enquiry may be held and how they are arranged are significantly different).
There are certain cases where a coroner is obliged to hold an inquest even when the death is from natural causes, such as when someone has been in state detention e.g. under arrest or in prison, at the time of death.
The coroner will usually open the inquest in order to issue a burial order or cremation certificate as well as hearing evidence confirming the identity of the deceased. The inquest will then be adjourned to be resumed at a later date. When the coroner's investigations are complete, a date for the inquest is set and the people who need to know will be told. Under some circumstances, it may take many months, or even years, for an inquest to be held. Inquests are open to the public and journalists are usually present.
Inquests are not permitted to determine blame and the conclusion (verdict) will not identify someone as having criminal or civil liability.
If police charge someone with causing the death, the inquest will not be resumed and the family will be informed of the arrangements made to register the death. This is to avoid two different courts examining the same evidence.
Inquest is a charity providing free advice to bereaved people facing an inquest, with a focus on deaths in custody.
Will the funeral and probate have to be delayed?
If a coroner decides an inquest is necessary it does not mean that all the practical issues have to be delayed until the inquest is complete. The investigations for inquests can sometimes take weeks or even months depending on the complexity of the case. Changes are coming to the coronial service that will aim to release the body for the funeral within 30 days wherever possible and to complete inquests more rapidly.
As well as issuing permission for the funeral to go ahead, the coroner can issue an interim death certificate (also known as an interim certificate of the fact of death), which can be used to notify asset holders and other organisations of the death and to make an application for probate. A grant of probate or letters of administration can be obtained and the estate distributed. However some insurance companies will not pay out from any policies held in case the circumstances of the death makes the policy invalid, e.g. if the person who died took their own life.
If police are investigating a death in suspicious circumstances, this may also delay distribution of an estate because a beneficiary will be disqualified if they are convicting of causing the death.
Support at Coroners' courts
The Coroners' Court Support Service is designed to give practical and emotional support to people attending a Coroners' Court.
When is an inquest needed?
If the cause of death remains in doubt after a post-mortem examination and further tests are required, or if it is determined that the death was not from natural causes, an inquest will be held (in Scotland a ‘fatal accident inquiry' although the circumstances in which a fatal accident enquiry may be held and how they are arranged is significantly different).
There are certain cases where a coroner is obliged to hold an inquest even when the death is from natural causes, such as when someone has been in state detention e.g. under arrest or in prison, at the time of death.
The coroner will usually open the inquest in order to issue a burial order or cremation certificate as well as hearing evidence confirming the identity of the deceased. The inquest will then be adjourned to be resumed at a later date. When the coroner's investigations are complete, a date for the inquest is set and the people who need to know will be told. Inquests are open to the public and journalists are usually present.
Inquests are not permitted to determine blame and the conclusion (verdict) will not identify someone as having criminal or civil liability.
If police charge someone with causing the death, the inquest will not be resumed and you will be informed of the arrangements made to register the death. This is to avoid two different courts examining the same evidence.
Will the funeral and probate have to be delayed?
If a coroner decides an inquest is necessary it does not mean that all the practical issues have to be delayed until the inquest is complete. The investigations for inquests can sometimes take weeks or even months depending on the complexity of the case.
As well as issuing permission for the funeral to go ahead, the coroner can issue an interim death certificate (also known as an interim certificate of the fact of death), which can be used to notify asset holders and other organisations of the death and to make an application for probate. A grant of probate or letters of administration can be obtained and the estate distributed. However some insurance companies will not pay out from any policies held in case the circumstances of the death makes the policy invalid, e.g. if the person who died took their own life.
If police are investigating a death in suspicious circumstances, this may also delay distribution of an estate because a beneficiary will be disqualified if they are convicting of causing the death.
Tell Us Once is a service offered by most register offices, by phone and on-line (with the reference number given by the local registrar when the death is registered) which helps with the practical tasks following bereavement by taking on the role of informing any government department with which the deceased had dealings before their death. The service allows the bereaved person to inform central and local government services of the death at one time rather than having to write, telephone or even attend each service individually.
Other practical tasks for the executors include starting the procedure for obtaining a Grant of Representation from the Probate Office in order for them to administer the estate of the person who has died. This may involve the paying of inheritance tax.
Most banks and public utility companies have special departments with trained staff to make notifying them of a death as simple as possible. Details are usually revealed by a search of 'bereavement' on the company's website.
People who have been widowed may be entitled to a Bereavement Payment and widowed parents are entitled to Widowed Parents Allowance. Both of these are likely to change in the future under clauses in the current Pensions Bill concerning Bereavement Support Payments but current arrangements are outlined on the Government's information site (gov.uk).
The Government (gov.uk) website has information on what needs to happen after a death.
If a death occurs abroad, the death needs to be registered according to the local regulations of that country and a Death Certificate should be obtained.
Circumstances will differ depending on whether there is someone who was with the person when they died who can make arrangements for both registration and repatriation or if arrangements need to be made at a distance/from the UK.
The Government produce a leaflet (see link below) that explains in what ways the Consulate Service can help with arrangements and with making contact, where necessary in the right language, with officials. It also explains some of the challenges involved in carrying out the deceased person's wishes (for example, if cremation facilities are not available in the country where they died).
If family or friends were with the person abroad when they died, they may be able to access support through the Consulate service or travel company representative.
Once a Death Certificate (or an authorisation for the removal of the body if there are ongoing investigations into the death) has been obtained, circumstances vary on whether the deceased person's body is to be repatriated or if a burial or cremation is to be held abroad.
To bring a body or ashes back to England or Wales, either the Death Certificate or an authorisation for the removal of the body from the country of death by someone authorised to do so are required. Then, to arrange a funeral in England or Wales, the following are required:
To arrange a cremation, a cremation order from the Home Office or a form E from the coroner will be required. If the death was from natural causes, the Home Office will require the following documentation;
If the death was not natural it will be referred to the coroner in the district where the deceased person was most recently living who will open an inquest to investigate the cause and circumstances of death.
A firm of funeral directors in the UK will have experience and be able to assist with repatriation of either the deceased's body or ashes.
Repatriation for a funeral overseasIf the funeral will be taking place abroad, there are certain legal requirements that need to be fulfilled.
If a body is to be moved abroad, the Coroner for the district in which the deceased person's body currently rests should be notified and should complete a Removal Notice (form 104). Often this authorisation has to be requested at least 4 days before the person is to be moved to give time for any enquiries.
Many countries require signed documents from an appropriate doctor that the deceased was not suffering from any condition that might pose a public health risk.
Repatriation may mean additional costs, for example caskets and embalming for repatriation have to conform to high specifications as well as the cost of the flight itself and costs of storage and transportation in the destination country. A less expensive alternative is to have the cremation in this country with repatriation of the ashes/cremated remains.
Cremated remains may be carried to some countries in hand luggage (with a death certificate and a certificate from the crematorium and sometimes a consular seal) but each nation has its own regulations.
Any funeral director can organise repatriation and advice on choices; some specialise in this type of work and have expertise in particular countries and airlines. Consulate services for the destination country should be able to advise on all procedures.
www.gov.uk/government/uploads/system/uploads/attachment_data/file/35526/bereaved-families.pdf
www.gov.uk/government/uploads/system/uploads/attachment_data/file/193657/Death_Overseas_web_13.pdf
Every year hundreds of people die while waiting for a transplant. Receiving a transplant of an organ or tissue can transform the life of a chronically ill person. Such transplants depend entirely on the generosity of donors and their families who are willing to make this life-saving or life-enhancing gift to others.
Many people who have received a life-threatening donation may consider organ and/or tissue donation, if medically appropriate. The NHS website for organ and tissue transplants contains links to online registration of consent. It is important that registration on the donor register is shared with family and friends and with medical staff.
"I want you to know that I have added my name to the NHS Organ Donor Register so that I can help someone else to live after my death."
After a sudden death, it can be difficult for medical staff to approach families who are still in shock to ask about organ donation. If asked sensitively, many families feel that this is something their relative may have already chosen or would choose: a way of continuing to make a contribution to someone else's life.
Whilst only a small number of people are able to donate organs and/or die in circumstances where their organs can be donated (normally within a hospital while on life support machines), many more are able to donate one or more tissues after death. Organs such as kidneys, heart, liver, lungs, pancreas and the small bowel can all be donated for transplantation. Tissues that can be donated include: heart valves, skin, bone, tendons, cartilage and corneas. Tissues can be donated up to 48 hours after a person has died, with the exception of corneas which must be retrieved within 24 hours.
www.organdonation.nhs.uk/about_us/professional_development_programme/
In some areas, hospice care is available from trained professionals and volunteers in a person's own home. This has the advantage of care from those who are trained to provide it within the comfort and familiarity of home surroundings. The National Association for Hospice at Home provides a directory of local services.
As part of Advance Care Planning, people usually express a preference on where they would like to die if their death is expected. For the majority of people this is in their own home – with appropriate care and support; although others feel they and their family will feel more supported in a hospice or hospital setting. In practice, just over half the people who die each year, die in hospital.
Palliative care teams, following the Gold Standards Framework, are committed to supporting a person to die at home if this is possible in terms of the equipment and medication required and the degree of medical support required. Everyone facing death will need some supportive care in addition to their treatment; in some cases this may involve 24 hour care. This would place a huge strain on families and friends and may not be possible if there are no supportive family members or friends available.
The following all have a role to play in supporting a person who wishes to die at home
www.dyingmatters.org/page/planning-ahead#where
www.mariecurie.org.uk/en-GB/nurses-hospices/nursing-in-your-home/care-at-home/
www.macmillan.org.uk/HowWeCanHelp/Nurses
www.gmc-uk.org/guidance/ethical_guidance/end_of_life_contents.asp
People involved in delivering end of life care should adopt an agreed, consistent approach and attitude to end of life care that encourages and accepts patient choice, regardless of their own background, culture and views. The National Institute for Clinical Excellence (NICE) has a quality standard based on acknowledging diversity and practicing equality: it describes the care that people approaching the end of life and their families and carers should receive that takes into account their preferences, regardless of their individual circumstances, including:
www.nice.org.uk/guidance/qualitystandards/endoflifecare/EqualityAndDiversityConsiderations.jsp
www.gov.uk/government/organisations/cabinet-office/about/equality-and-diversity
People involved in caring for people who have life-threatening or terminal illness have developed 'pathways' with accompanying quality of care standards to ensure that the most appropriate care and support is offered to the person and their family and friends at the right time and in the right way.
The 'Liverpool Care Pathway' or LCP was the most used guide for care in the last days; however, this is currently undergoing review and being phased out after some concerns were raised about how some people may have interpreted the guidance provided. Links below provide up-to-date information about the LCP and about the Leadership Alliance for Care of Dying People.
The likely emphasis in the future is not to have a 'Pathway' as such, but to tailor response at the end of life to the needs and best care of individual people.
Other supportive care pathways (SCP) have been developed and are in operation. One example is the SCP developed by the Sandwell and West Birmingham NHS Trust. Like all such pathways, its underlying aim is to identify dying patients promptly and improve the quality of end of life care by providing a focus on end of life issues and ensuring the multidisciplinary team is closely involved at every stage. The pathway is not prescriptive and does not curtail any care that would benefit the patient. However, because it is an end of life care pathway, it will direct the team to consider comfort measures as a priority.
Local NHS Trusts can provide information on their own Supportive Care Pathway.
www.england.nhs.uk/wp-content/uploads/2014/01/lacdp-interim-statement.pdf
Organisations offering support to people at the end of their life, and to their family and friends. need to have in place end of life care strategies, core policies, training and education programmes as well as knowledge of alternative sources of help and support.
Society in general can play a part by encouraging everyone to think about end of life choices.
A Will is a legal document in which you specify what you would like to happen to your estate, which includes all of your property, money and possessions. Whilst a Will is not a legal requirement, it is the best way to ensure your intentions are known and acted upon.
Some organisations run support groups where groups of bereaved people meet for mutual support. Some of these are 'open', meaning that people can join or leave at any time; others are 'closed' meaning that the group is planned around a set number of sessions and the same group starts and ends together. Some have a trained 'facilitator' or leader and others may be peer led and supported.
Cruse offers bereavement support both face-to-face and in groups.
WAY Widowed and Young offers support and friendship to those who have been widowed under the age of 50.
The Compassionate Friends (TCF) operates local support groups for those who have lost a child (of any age)
Survivors of Bereavement by Suicide (SOBS) operates local support groups for those who have been bereaved through suicide
Winston's Wish, Child Bereavement UK and other local child bereavement organisations provide groups for children, young people and their families who have been bereaved by suicide; for those bereaved through murder or manslaughter and for those bereaved through the death of a member of the armed forces.
Also, increasingly, people are finding support through online 'groups' and/or on message boards and web forums.
Care of a family when their baby dies in a maternity unit
Taking a baby home after death
Taking photographs following the death of a baby
When an adult is dying or has died: considering children
Breaking bad news to children: information for staff
Talking to children when a baby dies
Involving children when a parent is not expected to live
Involving children when a parent is on ITU and not expected to live
After a death, family and friends should be offered information about community bereavement services. In some cases, people may be reluctant to ask for help and it can be helpful to have contact established automatically by those who have offered support around the time of the death.
Community bereavement services may be offered by:
In medicine, nursing and the allied health professions, end-of-life care refers to health care, not only of patients in the final hours or days of their lives, but more broadly care of all those with a life-threatening or terminal illness or terminal condition that has become advanced, progressive and incurable. The term can sometimes also be used for the last care of someone who has died suddenly.
End of Life Care StrategyThe End of Life Care Strategy, published by the Department of Health in 2008, identified a number of significant issues affecting dying and death in England:
The strategy promotes high quality care for all adults at the end of life in England by providing people with more choice about where they would like to live and die. Similar strategies for the end of life have also been developed in Wales, Scotland and Northern Ireland.
Each year, just over half a million people died in England, about 99% of them adults over the age of 18, and almost two-thirds adults over the age of 75. About three-quarters of deaths could be considered "predictable" or expected and follow a period of chronic illness – for example heart disease, cancer, stroke or dementia. In all, around 58% of deaths occurred in an NHS hospital, 18% at home, 17% in residential care homes (most commonly for people over the age of 85), and about 4% in hospices. However a majority of people would prefer to die at home or in a hospice, and according to one survey less than 5% would rather die in hospital. A key aim of the strategy therefore is to reduce the needs for dying patients to have to go to hospital and/or to have to stay there; and to improve provision for support and palliative care in the community to make this possible. One study estimated that 40% of the patients who had died in hospital had not had medical needs which required them to be there.
The steps one to six are part of End of Life Care Planning and are followed in staff training.
Staff and volunteers should feel able to talk openly and honestly with people at the end of life and with their family and friends: this will include being able to recognise and use triggers for these discussions.
See details of core skills in the document.
Those involved in offering support should be able to hold conversations about advance planning for end of life care with patients and their families, demonstrating understanding of the various factors and influences that can affect an individual's end of life choices. This will also involve helping a person complete an Advance Care Plan which is regularly reviewed.
See details of core skills in the document.
All staff and volunteers should be aware of and use the additional resources of the community and voluntary sector to provide people at the end of life and their families, friends and carers with co-ordinated support.
See details of core skills in the document.
All staff and volunteers in whatever setting (hospital, hospice, home) should be aware of the appropriate care for people in their last days and hours and deliver this care with sensitivity and respect.
See details of core skills in the document.
All staff and volunteers in whatever setting (hospital, hospice, home) should deliver consistently high-quality care to people at the end of life and their families, friends and carers.
See details of core skills in the document.
Medical and nursing staff will usually know when the final stages are approaching. Physical signs of deterioration will be noted and the person's care adjusted to fit these conditions.
This will be a time when it is important to check if the person has expressed specific wishes about what they do and do not want to receive in treatment in the last stages of their life. (see Advance Care Planning). It is also the time to consider the level of pain control.
This is also the time for family and friends to be informed (if not already) in clear language that death is imminent. It is important that children and young people are included in this sharing of information. Families appreciate hearing this news from someone who has already been involved with their relative's care.
The person who is deteriorating will have emotional needs which need attention as well as physical ones; they may be afraid, have regrets and needs – or they may experience a sense of calm and readiness.
www.gmc-uk.org/guidance/ethical_guidance/end_of_life_contents.asp
All staff and volunteers who work with people with life-threatening conditions and/or within emergency departments should receive training in talking confidently and clearly with patients and their families and friends.
At the basis of high quality care for patients and their families is the need for communication: between patients and their medical teams; between families and those caring for the deceased person (whether over a period of time if the death is expected or under the pressure of explaining a sudden death); within families; between families and the services that offer support after a death.
Guidance on how to communicate with the dying, their families and the bereaved can be found within the links under 'education' and 'training'.
Key principles include:-
The website 'Breaking Bad News' is designed to help communication with people with intellectual impairment; however its tips and guidance are useful in any situation.
The person who is dying may want to talk about what is happening but be unsure whether their family can cope with the truth. Their family and friends may want to talk but do not want to distress the person who is dying. This can develop into a 'protection racket' with both sides wanting to discuss the situation and neither daring to start. For help with starting these conversations, please see the links below.
www.dyingmatters.org/page/TalkingAboutDeathDying
www.winstonswish.org.uk/mainsection.asp?section=000100010002&pagetitle=Parents%2FCarers
Around a quarter of all deaths in the UK are sudden or unexpected. Causes include: heart attacks, brain haemorrhages, accidents (including road traffic incidents), suicide, murder and manslaughter. In addition, many people with chronic and life-threatening conditions may die 'suddenly' even if their death has been predicted.
A sudden death brings severe shock and distress to family and friends yet is often experienced within a busy A&E or other unfamiliar situation. These circumstances make it simultaneously more difficult for staff to provide appropriate space, time, quiet and understanding and even more important for these needs to be met.
The provision of bereavement support from bereavement service personnel within the hospital should be rapidly arranged. Some voluntary organisations provide support for those who have been bereaved suddenly.
Ideally, all hospitals should have facilities where family and friends can be with the person who has died suddenly, away from other distractions.
When death has been through violence or accident, there may also be police involvement, even within A&E. This can be disconcerting, at the least, to families and staff can play a role in encouraging a subtle presence.
National Association of funeral directors: www.nafd.org.uk
Ministry of justice: www.justice.gov.uk
Department of health end of life care: www.dh.gov.uk
There are several kinds of specialist nurses who can support people who are dying at home. These may be provided by:-
www.nahh.org.uk/about-hospice-care
www.mariecurie.org.uk/en-GB/nurses-hospices/nursing-in-your-home/get-a-marie-curie-nurse
www.macmillan.org.uk/HowWeCanHelp/Nurses
www.helpthehospices.org.uk/about-hospice-care/find-a-hospice/uk-hospice-and-palliative-care-services
Wherever the person is dying, it is important for them and for their families to continue to have access to their consultant (or the nominated registrar).
As a person nears death, it continues to be important for the consultant to communicate clearly with the family and to have overall responsibility for ensuring that the patient's wishes are balanced with what will provide them with the greatest comfort.
www.gmc-uk.org/guidance/ethical_guidance/end_of_life_contents.asp
There is a wealth of information on the web to support decisions at the end of life. Please see specific links elsewhere on this pathway.
www.gmc-uk.org/guidance/ethical_guidance/end_of_life_contents.asp
It important that all services and individuals providing support both before the end of life and after bereavement, have sensitivity and insight to cultural and religious requirements. Information on different faith practices around a death and in mourning should be familiar to staff and volunteers and/or easy to access on demand.
It is also important to remember that there is a wide difference of beliefs and practice within faiths and cultures – and within families. It is always appropriate gently to ask what forms of care would be appreciated and when.
Those providing care after a death need to be aware of traditions associated with the treatment and disposal of the body of the deceased person and the likely difficulties for some cultures if, for example, a post-mortem and/or inquest is required and the funeral delayed.
The Multi-faith Group for Health Care Chaplaincy has resources and information on its website.
Health care chaplains within the NHS can access faith-appropriate support (including secular/humanist support) for patients and their families.
It is also important to remember that there are many types of culture, not all of which are based around belief or ethnicity. For further reading on this:
Death and Bereavement across Cultures: Murray Parkes C. (editor); Routledge; 1996
On Bereavement: Culture and Grief : Walter T.; Open University Press; 1999
www.mfghc.com/resources/resources_faithindex.htm
The last offices are the procedures performed usually, in the developed world, by a nurse, to a dead person shortly after death has been confirmed. They can vary from hospital to hospital, and culture to culture. It is important that, wherever possible, a person's faith and cultural practices are followed. The need for post mortem examination may make it impossible to carry these out.
Last offices should be performed when family and friends choose, whenever possible. They may wish to spend time with their relative's body after death before any practical care takes place.
Each hospital or hospice will have guidance on Last Offices. The procedure typically includes the following steps, though they can vary according to an institution's preferred practices.:
www.nhsiq.nhs.uk/media/2426968/care_after_death___guidance.pdf
All deaths must be confirmed or verified by a suitably trained person. This is usually a doctor or a nurse who has undergone appropriate training. The purpose of verification is to confirm that the person has died. The person carrying out the verification may not be able to issue the Medical Certificate of Cause of Death (Death Certificate).
Certification can only be carried out by a registered medical practitioner (that is, a doctor) who looked after the patient during their last illness.
The Academy of Medical Royal Colleges has a comprehensive code of practice for the diagnosis and confirmation of death.
The body of the deceased person should be cared for in a dignified and culturally sensitive way. Some cultures and faiths have requirements for how the body should be treated which should be followed wherever possible. The deceased was once a unique, living person and should continue to be treated with respect and dignity. The NHS Improving Quality website carries comprehensive guidance around the time of death.
It is important to remember and be sensitive to the needs of family and friends – there is no great rush, for example, to clean or move the body. Equally, it may make staying with a loved one's body easier if it has been cleaned and prepared for viewing.
It may be easier to take time caring for the deceased patient if they have died at home, in a hospice or nursing home; hospitals may have pressure on bed spaces, however sensitive staff wish to be to meet the needs of families and friends.
Family and friends may appreciate helping to clean, arrange and dress the body after death.
www.nhsiq.nhs.uk/media/2426968/care_after_death___guidance.pdf
Immediately after a death, especially when a death has been sudden, families may struggle to remember information. It is therefore important to provide this in several formats, both verbally and in written form, with options to website information.
Information provided can be of two types: that relating to practical tasks and that relating to where to access emotional support after a death. Equally, there should be information about what has happened, what tasks next need to be carried out and where further support can be accessed.
There are also many people who will need to be informed of the death. You can find more information about letting people know in this section.
One of the first things that need to happen when someone has died is for the death to be registered. This process will depend on the location and nature of the death. To do this, a Medical Cause of Death Certificate needs to be produced; deaths almost always need to be registered in person.
The death must be registered by the registrar:
In England and Wales, it is possible to delay registration for a further 9 days provided that the registrar receives written confirmation that the medical cause of death certificate has been signed by a doctor.
The registration should be made in the district in which the death occurred (unless the death has occurred in a county that has adopted a county-wide system). If this is not possible, the death can be registered elsewhere through a process of 'declaration' – in this case, there is a delay before the Death Certificate is issued. In Scotland the registration may be done at any Scottish registration office.
Registrars may operate appointment systems. Some operate an emergency out of office hours service for families needing an urgent funeral for any reason (such as faith requirements).
In general, registration of the death should be carried out before the funeral can go ahead. Exceptions are deaths subject to investigation by the coroner or procurator fiscal. Permission for burial may also be issued before full registration in certain circumstances but this is not possible if cremation is planned.
Tell Us Once is a service offered by most register offices, by phone and on-line (with the reference number given by the local registrar when the death is registered) which helps with the practical tasks following bereavement by taking on the role of informing any government department with which the deceased had dealings before their death. The service allows the bereaved person to inform central and local government services of the death at one time rather than having to write, telephone or even attend each service individually.
www.nhs.uk/CarersDirect/guide/bereavement/Pages/Registeringadeath.aspx
A Medical Certificate of Cause of Death (usually simply called the 'Death Certificate') is a legal form issued by a medical practitioner who was involved in the care of the person during their last illness. Normally, the doctor will have seen the patient in the 14 days before the death occurred. The certificate records the medical diseases or conditions that led to the person's death and is required to enable the registration of the death to be carried out (except in cases where the Coroner arranges for a post mortem examination and/or inquest).
Where a cremation is to take place, additional medical documentation is required. These are referred to as the Medical Certificate (Form CR4), the Confirmatory Medical Certificate (Form CR5) and the Authorisation to Cremate Certificate (Form CR10). Form CR4 is often issued by the same doctor who completed the Medical Certificate of Cause of Death, but can be issued by another doctor who also cared for the patient during their last illness and has also examined the body after death.
Form CR5 is completed by a doctor independent of the treating doctors, who will need to discuss the circumstances of the death with the treating doctor and another person (often a nurse who cared for the patient or a member of the patient's close family). The final certificate, Form CR10 is completed by a third doctor, employed by the crematorium, who scrutinises all of the cremation paperwork before allowing the cremation to take place.
The current system for death certification and scrutiny will be changing, with a new role of Medical Examiner introduced. The reforms are explained on the gov.uk website (see link below).
Professional associations and bodies have their own codes of conduct which underpin service provision to ensure it is of high quality, safe, fair and reflective. Contact the appropriate association, a few of which are listed below, for their codes of conduct in end of life care and bereavement support.
General Medical Council : www.gmc-uk.org
Nursing and Midwifery Council : www.nmc-uk.org/Publications/Standards
Standards in Bereavement Care Services : www.cruse.org.uk/gold-standards
Bereavement Services Association : www.bsauk.org
Childhood Bereavement Network : www.childhoodbereavementnetwork.org.uk/policyPractice_guidelines.htm
National Association of Funeral Directors : www.nafd.org.uk/funeral-advice/about-us/code-of-practice.aspx
When a person is dying, ideally they should be with their choice of family and friends – or alone if that is their choice. They may have expressed their wishes in an Advance Care Plan.
Within the home or a hospice, it is possible for family and friends, including children, to have their chance to say goodbye to their relative. This is often remembered as a very special, precious time.
Within a hospital setting, especially if the person was not expected to die, it is equally important but challenging for staff to provide enough space, quiet and time for relatives to feel they have had a chance to focus on being with the person who is dying.
Medical staff will verify that a person is at the point of death, following recognised signs. These will include particular patterns of breathing; changes to skin colour (usually moving up the body from the feet) and to lips and nails; unresponsiveness; jaw dropping open.
The Academy of the Royal Medical Colleges produces guidance on the diagnosis and confirmation of death.
www.aomrc.org.uk/doc_details/42-a-code-of-practice-for-the-diagnosis-and-confirmation-of-death
www.gmc-uk.org/guidance/ethical_guidance/end_of_life_contents.asp
When someone has been bereaved, their own GP should note this for any future consultations. A simple reference to the person who has died can be greatly appreciated. Some GPs automatically arrange an appointment with a person who has been bereaved a month or so after the death to check on how they are feeling.
Sometimes bereavement is associated with physical health difficulties; bereaved people may be more prone to illness or to accidents.
Grief itself is not an illness; it is a natural response to the loss of someone important. Grieving people can't 'pull themselves together' or 'move on'. In time, they may feel as if they have been able to 'grow around' their grief without it, in any way, going away.
However, sometimes people who are mourning need some extra help and GPs may refer people who are grieving in ways that are risking their own health for some counselling support (for example, through the Improving Access to Psychological Therapies programme).
www.rcpsych.ac.uk/expertadvice/problems/bereavement/bereavement.aspx
Sometimes, people who have been bereaved feel isolated by their grief. They don't wish to 'burden' others and put a brave face on to the world. Sadly, there are still accounts of old friends who cross the road rather than speak to someone who has experienced the death of someone close. The WAY Foundation has a useful book called: 'If there's anything I can do…how to help someone who has been bereaved'.
Letters, cards and calls of condolence are always appreciated. And also sending these around the anniversary of the death or on the person who died's birthday can be very comforting to the recipient. Noting these dates can help the bereaved person feel less isolated in their grief and provide an opportunity to share memories.
It is really important that all those who know someone who has been bereaved keep their antennae tuned for what may be helpful. Bereaved people appreciate specific offers of help rather than the generic 'do ask if there's anything I can do to help'. Examples include: dog walking; ironing; weeding; help with the school run. The WAY Foundation has a useful book called: 'If there's anything I can do…how to help someone who has been bereaved'.
Faith CommunitiesIf members of the bereaved family were part of a faith community, they may find this community's support especially welcome. However, occasionally bereavement can trigger questioning of previously held beliefs and it is important that faith communities can understand and respect this.
SchoolsIf a child has been bereaved, it is important that their school is informed and also that the teachers and other staff at the school are confident in offering their support and understanding to bereaved pupils. Bereavement can affect a child's ability to concentrate and to learn; some consideration is given in public examinations if there has been a recent bereavement. Guidance for schools can be obtained from many places, including Cruse, Winston's Wish and Child Bereavement UK.
WorkplaceIf the bereaved person is working, they are entitled to a small amount of time off for emergencies involving a dependent (this includes time to arrange and attend a funeral). There is no statutory bereavement leave as such. However, many employers offer more generous bereavement leave on compassionate grounds, recognising that few people could operate in the work environment after a major loss. Details will be in contracts of employment/terms and conditions or can be discussed with HR departments.
Family, friends and the wider communityAt best, family, friends and the wider community form 'circles' of support around people who have been bereaved, allowing them to grieve in ways that are helpful to them, and supporting them when they feel ready to face the future.
www.wayfoundation.org.uk/Screen/HelpingSomeoneBereaved.aspx
www.wayfoundation.org.uk/Screen/WhatToSay.aspx
www.winstonswish.org.uk/schools-information-pdf-page
www.nidirect.gov.uk/time-off-for-dependants-compassionate-leave
When a diagnosis from a professional is clear that the person is at the point of death, with all clear signs evident, family and friends should be offered the chance to say goodbye and/or be present at the end of life. This is a time for maximum pain control, for as much quiet and privacy as is possible and for any ritual tasks required by culture and faith.
Professionals offering care at the point of death will aim to make the process as natural as possible while ensuring the person's comfort and respecting their final wishes as expressed in the Advance Care Plan. 'Allow natural death' is sometimes used as a way of saying 'Do not attempt resuscitation'.
The 'Liverpool Care Pathway' or LCP was the most used guide for care in the last days; however, this is currently undergoing review and being phased out after some concerns were raised about how some people may have interpreted the guidance provided. Links below provide up-to-date information about the LCP and about the Leadership Alliance for Care of Dying People.
The likely emphasis in the future is not to have a 'Pathway' as such, but to tailor response at the end of life to the needs and best care of individual people.
www.gmc-uk.org/guidance/ethical_guidance/end_of_life_contents.asp
www.england.nhs.uk/wp-content/uploads/2014/01/lacdp-interim-statement.pdf
When a person is dying, ideally they should be with their choice of family and friends – or alone if that is their choice. They may have expressed their wishes in an Advance Care Plan.
Within the home or a hospice, it is possible for family and friends, including children, to have their chance to say goodbye to their relative. This is often remembered as a very special, precious time.
Within a hospital setting, especially if the person was not expected to die, it is equally important but challenging for staff to provide enough space, quiet and time for relatives to feel they have had a chance to focus on being with the person who is dying.
If the death occurs at home or at a hospice, it is normally the GP or medical director who has been providing and monitoring the patient's care who will provide the death certification; normally they will need to have seen the patient within the previous fortnight. If the GP has been in regular contact, there is no need for an out-of-hours doctor who does not know the patient to attend to certify death.
www.gmc-uk.org/guidance/ethical_guidance/end_of_life_contents.asp
A post-mortem, also known as an autopsy, is the examination of a body after death. The aim of a post-mortem is to determine the cause of death.
Post-mortems are carried out by pathologists (doctors who specialise in understanding the nature and causes of disease). Post-mortems provide useful information about how, when and why someone died, and they enable pathologists to obtain a better understanding of how diseases spread. Learning more about illnesses and medical conditions benefits patients too, because it means that they will receive more effective treatment in the future.
A post-mortem examination will be carried out if it has been requested by:
A coroner is a judicial officer responsible for investigating deaths in certain situations (see below). Coroners are usually lawyers or doctors with a minimum of five years' experience. In most cases, a doctor or the police will refer a death to the coroner. A death will be referred to the coroner if:
The main aim of a post-mortem requested by a coroner is to find out how someone died and decide whether an inquest is needed. An inquest is a legal investigation into the circumstances surrounding a person's death.
Coroners are required by law to ensure a port-mortem is carried out if requested, families are unable to withhold consent for a coroner's requested post mortem although it may be possible to discuss religious objections to the procedure.
A coroner may decide to hold an inquest after a post-mortem has been completed. Samples of organs and tissues may need to be retained until after the inquest has finished.
If the death occurred in suspicious circumstances, samples may also need to be kept by the police, as evidence, for a longer period. In some cases, samples may need to be kept for a number of months or even years. The circumstances in which tissue can be held are determined by the Human Tissue Authority and should be discussed with families who may have strong feelings about the retention of any tissue.
Hospital post-mortem examinationPost-mortems are sometimes requested by hospital doctors to provide more information about an illness or the cause of death, or to further medical research. Sometimes, the partner or relative of the deceased person will request a hospital post-mortem to find out more about the cause of death.
Hospital post-mortems can only be carried out with consent. Sometimes, a person may have given their consent before they died. If this is not the case, a person who is close to the deceased can give their consent for a post-mortem to take place.
What happens during a post-mortemA post-mortem will be carried out as soon as possible, usually within two to three working days of a person's death. In some cases, it may be possible for it to take place within 24 hours. During the procedure, the deceased person's body is opened and the organs removed for examination. A diagnosis can sometimes be made by looking at the organs: some organs need to be examined in close detail during a post-mortem and these investigations can take several weeks to complete. The pathologist will return the organs to the body after the post-mortem has been completed. Once release papers have been issued, the body can be collected from the mortuary in preparation for the funeral.
What happens after a post-mortemAfter a post-mortem, the pathologist writes a report of the findings and, if the post-mortem was requested by the coroner, the coroner or coroner's officer will inform families of the cause of death determined by the pathologist. There may be a charge for the full copy of the report.
The results can be discussed with the doctor in charge of the deceased person's care while they were in hospital (if applicable), or with their G.P.
There should be opportunities after a death, particularly if the death was sudden or the cause was uncertain requiring a post mortem examination, for family and friends to see the medical staff involved in the care of the deceased person. This may be a hospital consultant or registrar, in which case the hospital Bereavement Office will make arrangements or it may be the deceased person's G.P. who can be contacted directly.
It can help with the early stages of grieving to have sufficient information to begin to understand what has happened and why. Feeling that questions have been carefully answered and facts shared can help a grieving person in the first steps of a new reality.
All those involved in the care of the bereaved family and friends, including children and young people, are committed to providing the most helpful support in the most timely and seamless ways.
The National Bereavement Alliance is an emerging group of organisations with a shared vision that all people have awareness of and access to support and services through their bereavement experience. Alliance members contribute to this vision through their own aims and objectives, in various ways and at various times. While highly diverse in the primary focus of their work, members share a common interest in support for bereaved people. The core membership of the Alliance comprises national and regional membership organisations with an interest in the field of bereavement care, national providers of bereavement care and local bereavement care providers which have no other means of being represented.
Recognising each organisation's contribution, Alliance members collaborate strategically to provide a collective voice representing the needs of bereaved people and those supporting them. Among current tasks are:-
Some people prefer to access bereavement support, at least initially, at a distance. Grief can be exhausting and it is hard actively to go out to seek help or even to receive a bereavement support worker into the house. Some may prefer the anonymity of telephone or email support.
Cruse offers free confidential support for adults, children and young people, and this can be by telephone on 08444 779400 or email on helpline@cruse.org.uk. There is a freephone number specially for children and young people on 0808 808 1677. Cruse has a website specifically for children and young people – rd4u.org.uk and emails can be sent to info@rd4u.org.uk.
Services for children can also be accessed through the website of the Childhood Bereavement Network or by calling the Winston's Wish helpline for anyone supporting a grieving child on 08452 030405 or emailing chris@winstonswish.org.uk or by calling the helpline of Child Bereavement UK on 0800 0288840 or emailing on support@childbereavement.org.uk
When despair or distress are particularly strong, especially if this happens after normal service opening hours, the Samaritans are available to listen 24 hours a day, every day of the year. Call 08457 909090 (01850 609090 in Ireland) or email jo@samaritans.org
One to one support / home visitsSome organisations, in particular Cruse Bereavement Care, can offer one to one support from trained volunteers in people's homes. Other local bereavement services may be able to offer one-to-one support from their centres.
Sometimes the natural process of grieving can become so severe that additional professional help may be necessary. The person's GP will be able to access support if this becomes necessary.
Information and signpostingThe Bereavement Advice Centre can offer information, advice and signposting on a wide range of issues. They can be called on 0800 634 9494 or emailed on info@bereavementadvice.org
The purpose of providing timely, seamless and high quality support at the end of life is for those on the 'receiving end' to feel that they retain a degree of control over their individual care and the choices that need to be made.
The purpose of providing timely, seamless and high quality support after a death is to walk alongside those who are grieving until such a time that they feel it is possible to live on without the person who has died into a changed but, ultimately, hopeful future.
The Mental Capacity Act 2005 is an Act of the Parliament applying to England and Wales. Its primary purpose is to provide a legal framework for acting and making decisions on behalf of adults who lack the capacity to make particular decisions for themselves.
The five principles are outlined in the Section 1 of the Act. These are designed to protect people who lack capacity to make particular decisions, but also to maximise their ability to make decisions, or to participate in decision-making, as far as they are able to do so.
Those who care for the dying (and their families) need to be aware of the Mental Capacity Act to guide their decision making. Put simply, the five principles can be stated as:-
The Department of Justice website contains links to all relevant documents.
www.justice.gov.uk/protecting-the-vulnerable/mental-capacity-act
When someone is very ill and when someone dies, life for their family and friends is changed for ever. The needs of children and young people used to be overlooked when planning family support but now many organisations can provide support before and after bereavement.
It can help for professionals to understand who most needs their support; this isn't always the obvious people. Best friends, for example, may find themselves on the sidelines of a funeral, making tea for little-known relatives.
There may be a change coming in public engagement with death. For a while it seemed to become a taboo subject, but now more people are talking about their own death and those of people they care about. Dying Matters is a broad based and inclusive national coalition of 30,000 members, which aims to change public knowledge, attitudes and behaviours towards dying, death and bereavement, and through this to make 'living and dying well' the norm. Organisations such as Final Fling and the Death Café movement are among those who are trying to normalise discussions about death and dying.
Communication between voluntary and statutory services in a locality, through cross-sector networks, is essential if the highest quality of service is to be provided to patients and their families and friends.
All services should have information in a variety of forms (written literature, web links, DVDs) and a variety of languages and text sizes on what support is available locally to different members of the family.
Signposting to, for example, community-based bereavement support may be the most helpful thing that can be offered but care should be taken to ensure that people do not feel too quickly passed across to another service. Equally, support offered at an early stage of the 'bereavement pathway' may have the best chance of helping in the long term and future.
At the basis of high quality care for patients and their families, is the need for communication: between patients and their medical teams; between families and those caring for the deceased person (whether over a period of time if the death is expected or under the pressure of explaining a sudden death); between families and the services that offer support after a death.
Guidance on how to communicate with the dying, their families and bereaved people can be found within the links under 'education' and 'training'.
Key principles include:-
The website 'Breaking Bad News' is designed to help communication with people with intellectual impairment; however its tips and guidance are useful in any situation.
The person who is dying may want to talk about what is happening but be unsure whether their family can cope with the truth. Their family and friends may want to talk but do not want to distress the person who is dying. This can develop into a 'protection racket' with both sides wanting to discuss the situation and neither daring to start. For help with starting these conversations, please see the links below.
The core of high quality care for the dying and for bereaved people is in responding to each individual and providing a service for that person and their circle of friends and family. This, of course, also needs to fit within the overall framework for the service provided.
To do this requires discussion and 'assessment' of what each person needs – physically, practically and emotionally. A starting point is to explore what is happening for this particular family at this particular time. What other events and challenges are adding pressure? What is their usual way of handling difficulties – to talk about it or to hide it away – as a family and as individuals? What support would each individual most benefit from receiving? How resilient are they usually? How supportive is their community?
Winston's Wish produce a guide to conducting assessments of a child's family after the death of a parent or sibling which can be easily adapted by services to other situations
The core of higAll those involved in the care of the patient before, at and after death, and in the care of their family and friends will be keen to co-ordinate and integrate their care in order to provide seamless support. This means that communication across teams and between statutory and voluntary sector providers in a locality is vitally important to good care of the patient and their family.
Ensuring regular meetings between local providers is one way to make sure this communication is happening.
After an unexpected death, it is important that family and friends are introduced in timely and thoughtful ways to the services that exist to support them.
Being alongside people's grief can lead to emotional strain, deep questioning and sometimes distress. Organisations offering support to those at the end of life and their families need to ensure that all staff and volunteers receive regular, focused support. The provision and acceptance of this support make it possible to offer better support to others. Making it an automatic part of service delivery ensures that people do not avoid receiving the support they need and deserve. All service quality markers will include provision of support and supervision to staff and volunteers.
Professional associations and bodies have their own codes of conduct which underpin service provision to ensure it is of high quality, safe, fair and reflective. Contact the appropriate association, a few of which are listed below, for their codes of conduct in end of life care and bereavement support.
General Medical Council : www.gmc-uk.org
Nursing and Midwifery Council : www.nmc-uk.org/Publications/Standards
Standards in Bereavement Care Services : www.cruse.org.uk/gold-standards
Bereavement Services Association : www.bsauk.org
Childhood Bereavement Network : www.childhoodbereavementnetwork.org.uk/policyPractice_guidelines.htm
National Association of Funeral Directors : www.nafd.org.uk/funeral-advice/about-us/code-of-practice.aspx
It is important for those supporting the bereaved in a professional capacity to have supervision to ensure that the help they are providing to those who are bereaved is of the highest possible quality. Anyone involved professionally (whether in a paid or unpaid role) should receive supervision from someone with the appropriate training; try contacting the appropriate professional body if this isn't currently on offer.
Research about the importance of supervision in counselling and therapeutic situations is available online.
www.bacp.co.uk/research/Systematic_Reviews_and_Publications/Supervision.php
Professional bodies (for example, Royal College of Physicians, palliative care teams) will provide training for staff in how to support for patients and families (including children) both before and after a death. Contact the appropriate body for more details.
There is a package on online e-learning resources for those involved in delivery end of life care, with some modules open of access for volunteers.
Education and training for members of community groups, including schools is provided by many bereavement organisations. Cruse Bereavement Care can provide bespoke training as well as a range of bereavement awareness courses.
Education and training for those who support children and young people facing the expected death of a parent or sibling and those who have been bereaved. A list of courses is available on the Childhood Bereavement Network website or contact local services through the CBN online directory. Training courses are also listed on the websites of Child Bereavement UK and Winston's Wish.
www.e-lfh.org.uk/projects/end-of-life-care
www.childhoodbereavementnetwork.org.uk/SubscriberEventsJanuary2014.htm
Professional bodies (for example, Royal College of Physicians, palliative care teams) will provide training for staff in how to support for patients and families (including children) both before and after a death. Contact the appropriate body for more details.
There is a package on online e-learning resources for those involved in delivery end of life care, with some modules open of access for volunteers.
Education and training for members of community groups, including schools is provided by many bereavement organisations. Cruse Bereavement Care can provide bespoke training as well as a range of bereavement awareness courses.
Education and training for those who support children and young people facing the expected death of a parent or sibling and those who have been bereaved. A list of courses is available on the Childhood Bereavement Network website or contact local services through the CBN online directory. Training courses are also listed on the websites of Child Bereavement UK and Winston's Wish.
www.e-lfh.org.uk/projects/end-of-life-care
www.childhoodbereavementnetwork.org.uk/SubscriberEventsJanuary2014.htm
If it is possible for a person to receive end-of-life care in their own home, it is usually necessary to also provide specialised equipment, such as adapted beds and oxygen. These will be arranged by the hospital or hospice providing the overall care in conjunction with the home care team.
It can sometimes seem abrupt for the equipment to disappear soon after a person has died, but such equipment is always in demand for other patients.